Twelve case studies show diet eliminated or improved rheumatoid arthritis symptoms.
Feedback from Rheumatoid Arthritis (RA) sufferers in my study found that it is often assumed by rheumatologists that diet changes will make little difference to the disease process for those with RA.
In this post I look at documented case studies where diet changes have eliminated or reduced symptoms of RA. I’ve given a summary of the studies as well as a chart with the findings. You will note that there is a range of foods that cause exacerbation of symptoms, and that these may be different for each person.
Important: RA is a complex disease, these documented case studies show successes, where RA is managed and symptoms reduced or even reversed in RA. This does not mean that RA can be cured. It does not mean that all people with RA will necessarily respond to diet. Overall the range of improvements to RA in diet studies was between 5 and 70% of participants. We also know that fasting ameliorates disease for almost all with RA. So diet matters, but finding trigger foods can be a time consuming process, and food triggers vary between participants.
Rheumatoid arthritis (RA) is the second most common form of arthritis in New Zealand estimated to affect 0.74% – 3.2% of the population or approximately 40,000 New Zealanders. It affects 3 times more women than men (Pezzullo, 2010). RA is a chronic complex systemic auto-immune disease characterised by severe inflammation of the synovial lining of the joints. This chronic inflammation causes pain, swelling, inflammation and stiffness of the joints, eventual destruction of cartilage and bone causing loss of function and joint deformity. RA severely affects mobility and quality of life. Rheumatoid arthritis also has many non-joint manifestations including inflammatory conditions in the lungs, eyes, skin, heart, brain and nerves (Scott, Wolfe, & Huizinga). RA is also associated with an increased risk of cardiovascular disease (Myasoedova & Gabriel, 2010), type 2 diabetes (Su, Chen, Young, & Lian, 2013) and osteoporosis.
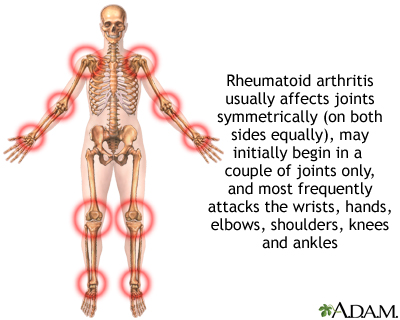
Joints typically affected in RA (source)
The Arthritis New Zealand website carries a brochure about nutrition and arthritis. Inside it states “Gout is the only type of arthritis that can be improved by changing your diet and lifestyle”. For those with RA “Do I need to avoid specific foods?” The answer is that although “Some people feel that cutting out acidic fruit such as oranges and grapefruit, and vegetables from the nightshade family, there is no scientific evidence that leaving out either of these foods does help and such diets may have he undesired effect of reducing beneficial nutrients” (NZ Arthritis, 2014)
Despite this information, many people with RA believe that diet can make an impact. In my research project I found around 45 case studies, intervention, and elimination diet studies specifically showing the impact of diet on RA.
Here is an overview of case studies of the effect of diet on RA
Twelve case studies from 1948 through to 2012 are presented. In most of these studies, problem foods were tested by eliminating and then re-introducing the to see what effect they had on symptoms.
Zeller (Zeller, 1948) presents 4 case studies. To identify potential food triggers for RA he took an extensive history of allergies, noting that “foods that were productive of other allergic symptoms often also cause arthritic symptoms.” He also notes that skin tests, both scratch and intradermal did not have value for finding trigger foods for RA, however positive tests were linked to other problems; allergic reactions like hay fever or rhinitis. Potential problem foods were identified, then excluded from the diet and tested with a challenge. He found the most effective diagnostic measure was food ingestion followed by white blood cell responses. Leukocyte counts dropped significantly over 40 minutes after problem food ingestion. Each person reacted to a specific food or foods, and once these were removed from their diets, symptoms resolved and measurements related to disease severity reduced, for example erythrocyte sedimentation rate (ESR). Zeller also noted that deformity and ankyloses reversed in two people over time. Foods identified in these four included milk (2), beef (2), eggs, pork(2), tomatoes, white potatoes, fish (2), banana, whiskey, beer, green beans, lettuce and nuts. Another observation of interest is the time to an inflammatory joint response after food ingestion. From the time food is ingested joint pain and swelling was noted as being 1 hour in case 1, 4-6 hours with maximum intensity at 16 hours in case 2, in case 3 response to milk was 45 minutes and other foods 3 hours, persisting for 24 – 36 hours. In case 4 pain, swelling and fatigue took 4 -5 hours persisting 36 hours.
Three case studies showed patients reacted strongly to a single food or food group and when the food was completely removed RA went into remission. The foods were dairy products; milk and cheese (Parke & Hughes, 1981), corn or maize starch (Williams, 1981), and cereals (Lunardi et al., 1988). Another case study identified milk as a trigger and this was confirmed with blinded testing (Panush, Stroud, & Webster, 1986). The patient went into complete remission whilst fasting or on Vivonex, an elemental liquid diet replacement. After milk ingestion it is notable that like the Zeller case studies, post ingestion symptoms began at 6 – 12 hours, peaking at 24 to 48 hours. Whilst this response time to a trigger is similar in these case studies, another case study of a 15 year old female with juvenile RA where dairy foods was confirmed as the trigger, response time was far slower, after eating dairy products daily in 4 separate challenges, she developed arthralgia, fatigue and arthritis in 10 to 23 days. Once dairy was removed symptoms resolved in 10 days to 3 weeks (Ratner, Eshel, & Vigder, 1985).
O’Banion used another method to find trigger foods in 3 case studies (O’Banion, 1982). Patients kept a food and drink diary, took their pulse hourly and recorded the severity of their arthritis pain and sleep quality. Two patients had elevated pulse rates after a number of foods. In the next phase the patients ate a diet which tested vegetables, meats and fruits one food per meal, 3 foods tested per day. Changes in pulse rate and joint responses were noted, this continued until a diet of non- reactive foods was found and patient was pain free. Food challenges continued and the most triggering foods were identified. All 3 reacted to dairy, wheat, cane sugar, corn and beef, and individually to a number of other foods.
The most recent case study (Denton, 2012) and the only one found after 1988, used a more modern elimination diet which removes common inflammatory foods. After a few days the patient’s pain reduced on this diet and food challenges began. Corn and nightshade vegetables were identified as trigger foods, once removed the patient went into remission and came off all medication.
| Study | Age F/M
Disease duration |
Diagnostic tests if known
/ symptoms |
Medication
used |
How foods that cause symptoms were diagnosed | Dietary treatment that reduced RA symptoms | Outcome of diet changes | Longer term | Food implicated as triggering RA |
| (Zeller, 1948) Case study 1 | Female, 39
9 years |
RA Joint symptoms
Fatigue Diarrhoea constipation Nausea Nasal congestion sneezing
|
Coal tar products partial relief | Elimination and food challenges
Symptoms exacerbated after ingestion of foods. Milk caused diarrhoea, nausea, headache & fall in leukocyte count 7400 to 5400 cells. Onset of joint pain, swelling from 1 hour. Chocolate and banana – headache. Beef, banana, fish, nuts on challenge produced fatigue, joint pain and swelling. Exclusion of foods gave relief of symptoms |
Exclusion of foods: milk, beef, banana, fish, nuts | Exclusion of foods produced relief of joint symptoms.
Ingestion produces reactions
|
Remains symptom free except for some finger swelling
ESR reduced from 20mm to 8mm/hour |
Milk, beef, banana, fish, nuts |
| (Zeller, 1948) case study 2 | Male, 67 25 years | RA Joint pain and swelling in hands, knees and ankles
fever fatigue |
“every therapeutic measure exhausted” | Patient observed whiskey and beer caused swelling and pain in joints.
Ingestion tests showed wheat, eggs, fish, tomatoes, pork produced joint pain and swelling and fatigue 4 – 6 hours post eating. Maximum intensity 16 hours before subsiding |
Exclusion of Wheat, eggs, fish, tomatoes, pork, whiskey , beer | On exclusion of foods, symptoms decreased 80% in 3 months
Ingestion tests at 3 and 6 months again produced symptoms |
2 years later some deformity and ankyloses reversed. ESR May 1946: 80mm/hr, March 1948 38mm/hr | Wheat, eggs, fish, tomatoes, pork, whiskey, beer |
| (Zeller, 1948)case study 3 | Female 41
6 years |
RA Joint symptoms, pain and swelling
Low grade fever Abdominal distension, wind, Cramps diarrhoea daily Sore throat |
Therapy ineffective
Salicylates, bee venom |
Ingestion tests (food challenges) with most frequently eaten foods
Pork – nasal congestion, abdominal bloating 40 mins Milk – coughing, fatigue, painful joints in 45 mins, sore throat, fever 3 hours. Diarrhoea during night. Lettuce, white potatoes, string beans, sore throat, joint pain and swelling 3 hrs, persisting 24 – 36 hours Exclusion of these foods resulted in remarkable improvement Deliberate ingestion causes symptoms |
Exclusion of Lettuce, white potatoes, string beans, milk, pork | Food exclusion “Remarkable improvement”
Deliberate ingestion causes symptoms |
Not known | Lettuce, white potatoes, string beans, milk, pork |
| (Zeller, 1948)Case study 4 | Female, white, 42
20 years |
RA Joint symptoms
Nasal congestion Pruritus ani headaches |
Not stated | Ingestion tests
Exclusion diet and re-introduction Ingestion tests: Milk: sneezing, headaches, in 20 minutes lasting 24 hours. Leukocyte count 5900 to 3900 cells in 40 mins. Wheat: sneezing in 15min, eggs- nausea in 5 mins (also leukocyte count drops 5400 to 4400 in 40min) Placed on exclusion diet with no reactive foods. Challenge with one food at a time, 2 days apart Beef- join pain & swelling, fatigue 4-5hrs, persisting for 36 hrs. Eggs, pepper, garlic – vaginal itching and eruption in 2 hours Pork, rectal itching Wheat, nasal symptoms Milk, nasal congestion |
Problem foods excluded.
Beef for RA, egg, pepper, garlic, pork, wheat, milk for other health concerns |
Not stated but assumed that no symptoms on exclusion diet | Deformity of hands disappeared,
Wheat was eliminated for 3 months now tolerated once day |
Beef only caused arthritis
Eggs, pepper, garlic -vaginal itching and eruption in 2 hours Pork, rectal itching Wheat, nasal symptoms Milk, nasal congestion |
| (Parke & Hughes, 1981) | 38, Female
25 years |
Erosive seronegative RA.
ESR 110mm/h Fatigue Dry eyes & mouth |
Salicylates NSAIDS, (not effective) prednisolone 10mg/d failed to relieve intense synovitis and stiffness | Elimination and
food challenge with milk and cheese
Inadvertent consumption of dairy, symptoms returned in 12 hours Monitored food challenge- in 24hours pronounced deterioration of arthritis, pronounced increase in synovitis, increase in Ritchie index, morning stiffness, 5mm increase in ring size, positive RAST to dairy IgE antibodies, heat-damaged red cell clearance rates |
Elimination of milk, cheese, and butter | In 3 weeks – decreased synovitis and morning stiffness. Improved Richie index, VPAS,
ESR Prolonged improvement in previously unresponsive RA |
Morning stiffness completely disappeared
Synovitis completely resolved “Well fully mobile, minimal residual disease activity.” Off prednisone |
Milk and cheese
|
| (Williams, 1981) | Female, age not known
25years |
“Active RA” pulmonary involvement | Aspirin, azathioprine | Removal of maize starch- dramatic improvement in 1 week
Accidental ingestion of corn-starch thickened gravy at 6 weeks “arthritis flared badly” |
Exclusion diet, elimination of corn and maize starch, including starch filler in medications | “Dramatic improvement” after 1 week of exclusion diet, off all medication. ESR fell from 75 to 31. Chest xray clear, lung function normal | Off all tablets
Looking and feeling better than ever Chest xrays clear, lung function ‘normal’ |
Maize / corn starch |
| (O’Banion, 1982) case study 1 | Female 21
7 years |
RA joint symptoms
Grand and petty mal seizures, headaches, fatigue, sleeping problems, depression, |
Dilantin for seizures, alcohol for pain | Diet reactions observed, followed by elimination diet and re-introduction of foods.
Phase 1: Patient recorded severity of arthritis pain 1- 10, pulse rate hourly and all food and drink consumed. Sleep quality recorded from 1 – 10 for 18 days. Phase 2: water only, testing of fresh fruit vegetables and meat, 3 foods tested each day, 1 food eaten at a time. 4 day rotation of foods. Food from same Biological family not eaten more than every 2 days. Reactions to foods noted – physical and behavioural When 3 pain free days, returned to normal diet to test. Day 44 normal diet resumed: result – pain returned to baseline levels within 7 to 10 days Resumed non-reactive diet of meats, vegetables, fruits. On return to non-reactive food diet became symptom free in 11 days Day 88 tested commercial and organic pork immediate and severe arthritis pain |
Treatment diet: Vegetables, meats and fruits, “non-reactive foods”
Tolerated foods: Apples, pears, watermelon, grapes, peaches, pineapple, carrots, lettuce, celery, cabbage, tune, eggs, green beans, salmon, crab , shrimp, walnuts, brazil nuts, coconuts, sunflower seeds avocado, sesame seeds |
Pain elimination 19 days into diet testing and elimination. She reported sleeping ‘sleeping extremely well’
Daily pulse rate decreased |
Patient had remained pain-free for 1.5 years, pain free at time of report. | She consistently reacted to: peanuts, beef, pork, oranges, dairy products, poultry, wheat, honey cane sugar, potatoes, coffee, corn barley, pecans.
Glue and paint fumes triggered epilepsy. |
| (O’Banion, 1982) case study 2 | Female 18years
8 years |
RA, primarily knee pain, periodically other joints.
Also headaches, temper, crying moodiness, confusion sinus problems, allergies. |
6 aspirin a day, minimal effect | Phase 1: Baseline data collected for 35 days. Diet response to food recorded eating normal diet.
Phase 2: day 36 – rotary diet fresh meats, vegetables and fruits. First symptom free day – day 9. Food testing- Irregular pulse or physical or behavioural reaction to that food noted. Reactive foods eliminated and questionable foods re-tested. Normal baseline diet resumed after 4 pain free days, result: pain returned to baseline levels No pulse rate changes to foods |
Elimination diet of meats, vegetables and fruits
testing for problem foods continued. Food removed permanently if caused a reaction |
Arthritis pain eliminated, reported sleeping well, not moody. Sinus discomfort and allergic symptoms completely eliminated. | Not stated | Wheat, beef, pork, cane sugar, milk, corn and a few other foods |
| (O’Banion, 1982) Case study 3 | Female 36
Duration not stated |
Periodic RA in several joints.
headaches, bowel disturbances frequent sleepiness, sinus problems, emotional problems, obesity. |
Phase 1: 13 day baseline data on normal diet
Phase 2: Testing and elimination day 14 to 32. Foods producing irregular symptomology eliminated Rapid decrease in pain, one test food cantaloupe marked increase in pain and pulse rate Phase 3: Day 33 normal diet resumed – this resulted in a gradual increase in pain. Reactive foods tested several times to confirm. Some foods consistently increased pulse by 10 – 20 beats/min which also caused physical and emotional responses |
Elimination diet of meat vegetables and fruits | No pain on day 32.
|
Not stated | Wheat, corn, tomatoes, cane sugar, milk products, eggs, apples, beef, lettuce, peanuts, cantaloupe, peas | |
| (Panush et al., 1986) | Female, 52, white
11 years |
Class I stage I, active disease. MSD 30 – 60 min, 9 tender joints, 3 swollen joints, objective assessment 87% on normal diet
ESR 27 – 42mm/hr |
Vivonex meal replacement and food challenges
Un-blinded challenge noted exacerbations with milk, beans, meat Normal diet 6 days- 30 min MSD, 9 tender joints, 3 swollen joint 87% subjective assessment Vivonex 2 days, fasting 3 days, No MS, swollen joint score 0, tender joint 1, assessments 100% Vivonex 33 days – no symptoms Blinded milk challenge – MSD 30 min, 14 tender joints, 4 swollen joints, objective assessment 80%, symptoms began 6 – 12 hours peaking at 24 – 48 hours. IgG and IgG4 anti-milk level increase marked. Beef, chicken, rice challenge was possible reaction but unclear |
Fasting, Vivonex Vivonex meal replacement 33 days | Fasting or Vivonex – no symptoms of RA
|
Not stated | Milk.
Shellfish – urticaria |
|
| (Lunardi et al., 1988) | Not stated | Serum positive RA ARA criteria
High IgE ESR 120mm/h Pleuritis, vasculitis, cutaneous ulcers
|
Methylprednisolone 24mg/die 10m
Gold salts 6mg/die Penicillamine 200mg/die 3m Clinical condition worsening |
Positive skin prick for cereals
3 week elimination diet then Challenge test: cereals triggered arthralgia, articular tumefaction, morning stiffness, vasculitis |
Removal of cereals from diet
|
Patient went into remission ESR fell to 20mm/h
Waaler Rose and Rheuma test negative (now known as Rheumatoid factor) Total IgE became normal |
1 year still in complete remission | Cereals |
| (Denton, 2012) | Female 65
15 years |
RA, gastritis, eczema, rhinitis, dry eyes, anxiety, poor sleep
fatigue |
Medication not effective, methotrexate produced side effects.
Trazadone for sleep tramadol |
Elimination and food challenge
Modified Elimination diet removing most common causes of inflammation – wheat, corn, cow’s milk dairy products, nightshade vegetables (white potatoes, tomatoes, eggplant, peppers) followed by food challenges Improvement reported after a few days. More energy, bowels normalised, pain ‘dramatically reduced’ On re-introduction corn caused eye dryness, joint inflammation and colitis. Nightshades – burning pain in back, arms, and hands, very achy, plus bloating and nausea. No reaction to cow’s milk or wheat |
For next 5 months avoided all corn and nightshade vegetables | Completely off methotrexate, trazadone and tramadol. Able to do treadmill training | Able to go on hiking trip to Asia. | Corn, nightshade vegetables (white potatoes, tomatoes, eggplant, peppers) |
This research gives hope for the people with RA!
Does everybody respond the same way to the trigger food? I mean, will I necessarily feel worse if I eat some tomatoes?
Everyone is different. When an elimination / reintroduction diet is done – people discover they react to some things and not others, when they reintroduce that food. For yourself, you will only figure it out using this method. Hope this helps. Julianne
As someone who has been living with rheumatoid arthritis for several years, I have learned that certain foods can trigger flare-ups and exacerbate my symptoms. While trigger foods can vary from person to person, I have found that there are some common culprits that I try to avoid.
One of the biggest trigger foods for me is sugar. When I consume high amounts of sugar, I notice that my joints become more inflamed and painful. I have also noticed that processed foods, which often contain added sugar, can trigger my symptoms as well.
Another trigger food for me is dairy. When I consume dairy products, such as milk or cheese, I often experience increased joint pain and stiffness. I have found that switching to plant-based milk alternatives, such as almond or oat milk, can help to reduce my symptoms.
I still consume sugar, and dairy, but in small amounts. To avoid it altogether, would mean missing out on some of life’s edible luxuries. Controlling my diet, and exercising, means I only need NSAIDs, not painkillers, on a daily basis. It has taken 30 years of my own research to get to this stage.
Thanks for sharing your experience. Yes dairy and sugar show up regularly in the clinical studies as being triggers for RA in many.